Several years ago, I developed intermittent bouts of what I would later term brain fog in which I experienced nonlucid moments, similar to waking up after anesthesia. The first and most memorable of these occurred while I was driving on I-565 to work one morning. While not exactly dizzy, I recall feeling so strange that I pulled the car over on the interstate and waited for the spell to pass. After a few minutes, the episode subsided and I went on with my busy day, forgetting about the strange incident. Months later, similar spells began occurring more frequently, heightening my preexisting hypochondriac tendencies that I had developed from years of reading medical books and watching TV programs about the rarest medical conditions in the world.
The spells would come on suddenly, without warning, and felt like a cloud engulfing my consciousness. I had a really hard time explaining the symptoms to my family practitioner at the time. “You know that feeling… where you’re having a dream… and then you start to fall… but then you don’t fall… but the ground is moving… and your thoughts don’t come as crisply or clearly…” Gosh, I sounded crazy even to myself. I further tried to explain that words sometimes did not come easily, decision making became more difficult, and my concentration span seemed shortened. After some routine blood work, I was reassured that my symptoms were likely from fatigue with an added dash of anxiety. But something felt wrong. The foggy spells progressed and I began experiencing pressure in my head, although the entire myriad of symptoms remained very non-specific.
Being in my late 20s and a medical provider with just enough medical insight into her own health to be unbiased, I did what any circumspect and logical person would do: I Googled it. After hours of pouring over medical articles, researching medical websites and reading the rantings of a few passionate bloggers, I settled on a very rational explanation for my symptoms…I had a brain eating amoeba. My family practice provider referred me to a neurologist where I was subjected (at my insistent request) to nearly every test known to man…MRI scans, toxicology, blood tests, nerve studies…you name it! The only time he laughed at me was when I asked him (only half-jokingly) if he would do a brain biopsy to make sure the large amounts of sushi I had been consuming hadn’t left an uninvited parasite swimming in my gray matter. The testing came back completely normal. No multiple sclerosis, no brain tumor, no lead poisoning, and certainly, no brain-eating amoeba. I was the picture of health.
Now, if you’re like me, there is nothing in the world more frustrating than knowing something is wrong and not having an explanation. What I’ve failed to mention thus far is that at this point in my life, I was working as an Ear, Nose, and Throat nurse practitioner, specializing in dizzy patients. As I continued to see patients day-after-day and listened to the way they described their symptoms, something clicked for me. My patients with inner ear conditions, specifically Meniere’s Disease, complained of dizziness, lightheadedness, vertigo and a feeling of being “foggy headed”. Eureka!But I wouldn’t describe my spells as dizziness exactly, more like a deviation from my normal clear thinking. About this time, I began noticing the pressure in my head was centered over my right ear and that I had developed a faint humming and roaring tone. Feeling a bit silly to have struggled for so long with what was quickly becoming a familiar ENT scenario, I asked our audiologist to check my hearing and run a simple sound test for Meniere’s Disease. It was positive in my right ear. Suddenly the brain eating amoeba had a name! But I had been treating patients with inner ear conditions for years and was completely oblivious to the fact that I had developed Meniere’s Disease! I laughingly tell my patients how I came to realize I had Meniere’s Disease. They too are generally relieved to have a diagnosis; especially one that is treatable. My best advice as a Meniere’s patient (and as their provider): STAY OFF GOOGLE! Dr. Google is the most dangerous physician in the world because he plays on the fears of uncertainty lurking in the dark parts of our (amoeba eaten) brain.
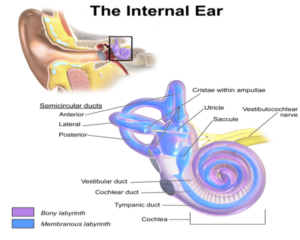
Meniere’s Disease is an inner ear condition usually characterized by dizziness, ear fullness, tinnitus (or noise in the ear), and hearing loss. You can have a combination of symptoms or all of the symptoms which can vary case-by-case. Meniere’s Disease is thought to arise from genetic and environmental factors, although the exact etiology is unknown. Pathophysiology is not fully understood, but thought to be related to a variety of events that lead to elevated pressure in the endolymph fluid causing a condition known as hydrops. Although dizziness can be Pandora’s Box in terms of differential diagnoses, inner-ear should always be a consideration once acute issues such as cardiac, vascular, and neurological conditions have been excluded. The history is critical. Find an ENT team (hint, hint) that will take the time to listen to your symptoms. Standard workup includes a hearing test (or audiogram) along with simple sound tests to measure inner ear pressure. Not to brag (cough, cough) but our practice recently upgraded to state-of-the-art inner ear test equipment that is second to none. As advances in technology continue to grow, we work closely with our audiological team to interpret results so that we can appropriately treat our patients.
Upon confirmation of a Meniere’s Disease diagnosis, treatments include initiating a low-salt, low-caffeine diet and medications such as diuretics, steroids, anti-nausea pills and drying agents (anticholinergics) depending upon the individual patient. Trans-tympanic steroid perfusion therapy offers a minimally invasive, in-office procedure that provides significant lasting relief for most patients. Some of the more invasive procedures and surgeries such as endolymphatic sac decompression should be reserved for more severe cases and are generally performed by board-certified neuro-otologists at universities in larger cities such as Birmingham and Nashville. Destructive procedures, such as gentamycin perfusions and labyrinthectomy can cause irreversible effects such as permanent hearing loss and are reserved for dire cases. (These are the Dr. Google recommendations we try very hard to stay away from). Most patients respond well to steroid perfusion therapy and rarely require further action. Balance therapy may be indicated for some, but for the majority of patients based on our clinical experience, this is generally not necessary.
Theories exist as to why a condition within the ear affects brain consciousness creating the sensation of fogginess. After pouring over the literature, my professional opinion is: no one knows. My personal opinion, having suffered this condition for many years, is that Meniere’s Disease creates a constant symptom of imbalance in which the body fights tirelessly to try to “right itself”. This constant exertion probably tires you, not only physically, but also mentally, creating a murkiness in your daily thoughts. Severity ranges from a mild brain mist all the way to a giant wall cloud.
Foggy-headedness can also arise from a number of additional medical conditions. Medications, migraine headaches, fibromyalgia, anxiety, sinus infections, allergies, multiple sclerosis, attention deficit disorders (and probably brain-eating amoebas) make the list. Accompanying symptoms such as nausea, vomiting, blurred vision, headaches, chest pain, syncope and of course ear symptoms will help your medical team zone in on which appropriate tests, procedures and referrals to order.
Many patients ask, “How do I fight the fog?” For me, achieving a low-salt, low caffeine diet (although I frequently cheat), and responding to ear steroid perfusions fought most of the battle. Staying physically active with aerobics such as, horseback riding, and waterskiing has also helped… not that I am graceful or even good at these activities! For older patients, other recommendations include walking, water aerobics, and staying active in general can help to improve vestibular function, physical health, and emotional wellbeing. I read (and write) as much as possible and practice sudoku puzzles to help improve my mental acuity. “Use it or lose it”, we often hear. Practicing mentally challenging activities has been helpful for me. I am often reluctant to tell patients how well I’ve done from treatments because I would hate for them to have a less effective result and compare themselves to my experiences. Nearly all of them appreciate the candidness and understand that each patient can have a different outcome. However, the vast majority of our patients do respond well to treatment and their quality of life improves vastly.
I am fortunate to work with one of the most knowledgeable ENT physicians in North Alabama. Dr. Neeta Kohli-Dang and I share a passion for diagnosing and treating dizziness in addition to a multitude of other ENT conditions. We’ve had numerous patients visit us over the years with symptoms similar to mine. When I was initially diagnosed, I was embarrassed that I had ignored my own signs of inner ear. What kind of a provider doesn’t realize she has the very condition that she treats? But after seeing Meniere’s patients for the majority of my nurse practitioner career, I’ve come to the realization that one size certainly does not fit all. I am able to chalk it up to the vagueness of my clinical presentation. Once clear-cut Meniere’s symptoms arose, I jumped on it like a duck on a June bug. And I certainly have no trouble telling my story, no matter how self-deprecating; if it helps someone lift the fog ????.
Written by Kari Kingsley, MSN, CRNP and originally published by Inside Medicine Magazine.
Kari Kingsley, MSN, CRNP is an otolaryngology nurse practitioner with over 10 years of ENT experience. She is a medical writing consultant for Inside Medicine and enjoys writing articles on pertinent material to keep the residents of North Alabama up to date at the forefront of medicine.